Chronic venous insufficiency (CVI) is a common circulatory disorder that impacts the veins in your legs. It occurs when the one-way valves inside your leg veins stop working properly, causing blood to flow backwards and pool in your veins.
This results in symptoms like varicose veins, leg swelling, leg heaviness, and leg ulcers. If left untreated, CVI can worsen over time and significantly impact your daily life.
The good news is that Medicare covers treatment for chronic venous insufficiency. There are effective options available to alleviate CVI symptoms, improve vein health, and prevent complications.
Based on our experience at The Vein Center Doctor, applying for Medicare coverage and utilizing the right treatments can greatly help in managing CVI.
Does Medicare cover the treatment of chronic venous insufficiency?
Yes, Medicare provides coverage for medically necessary treatment of chronic venous insufficiency. This includes diagnostic tests to evaluate your veins, prescription medications to manage symptoms, compression stockings to improve circulation, and minimally invasive procedures to treat faulty veins.
Specifically, Medicare Part A covers CVI treatment you receive as a hospital inpatient, like vein surgery. Medicare Part B covers outpatient care from doctors as well as preventive screenings, durable medical equipment like compression stockings, and vein procedures done in a doctor’s office.
For medications, Medicare Part D offers prescription drug coverage but there can be cost sharing. Finally, Medicare Advantage plans under Part C provide all Part A and B benefits along with prescription drug coverage.
What should I know about Medicare and chronic venous insufficiency treatment?
If you have CVI, it’s important to understand your Medicare benefits and how the program covers necessary vein treatment. Here are some key things to keep in mind:
- You will have out-of-pocket costs like deductibles, copays, and coinsurance for treatments, tests, and medications. Supplemental insurance can help cover these costs.
- Medicare covers CVI treatment that is deemed medically necessary by Medicare guidelines and your doctor. The Centers for Medicare & Medicaid Services (CMS) states that treatment of CEAP clinical classification C0 (no visible or palpable signs of venous disease) is considered cosmetic, and therefore, not covered.
- Some vein procedures and medications may require prior authorization from Medicare before they are covered. Your provider will handle this process.
- Using in-network Medicare providers lowers your out-of-pocket costs compared to going out-of-network.
- If Medicare denies a treatment as not medically necessary, you can appeal the decision and provide supporting documentation from your doctor.
Consulting with a vein specialist who understands Medicare guidelines can help navigate your coverage.
What Medicare options are available for chronic venous insufficiency treatment?

Medicare offers different plan options that provide coverage for CVI treatment:
- Original Medicare (Parts A and B) covers inpatient care, outpatient treatment from doctors, durable medical equipment, and procedures done in a doctor’s office.
- Medicare Advantage (Part C) offers all Part A and B benefits along with prescription drug coverage through private insurers. Many include extra benefits like vision and dental.
- Prescription Drug Plans (Part D) are standalone plans just for medication coverage. This helps cover CVI prescriptions.
- Medigap supplements Original Medicare by helping pay deductibles, copays, and coinsurance. These provide additional coverage for CVI treatment costs.
- Medicare-approved private fee-for-service plans allow you to go to any Medicare-approved doctor or hospital that accepts the plan’s payment terms.
Are there Medicare-approved treatments for chronic venous insufficiency?
The good news is that many treatments for chronic venous insufficiency are approved for coverage under Medicare provided they are medically necessary. Some of the main Medicare-approved options include:
- Compression stockings that apply gentle pressure to improve blood flow and reduce swelling. Medicare Part B may cover the costs for compression socks and stockings when they are directly related to treating a person’s venous stasis ulcer.
Our team at The Vein Center Doctor often recommends graduated compression stockings.
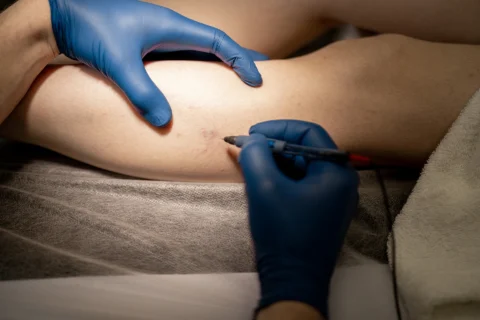
- Sclerotherapy injections delivered directly into varicose veins to shrink them.
- Endovenous laser ablation that uses laser energy to seal off damaged veins.
- Radiofrequency ablation that uses heat to collapse dysfunctional veins.
- VenaSeal closure that injects a medical adhesive to seal problematic veins.
- Vein stripping surgery to remove severely damaged surface veins.
- Prescriptions like pentoxifylline to improve circulation and manage symptoms. Medicare Part D covers prescription medications like pentoxifylline, which can help improve circulation and manage CVI symptoms.
How do I apply for Medicare coverage for chronic venous insufficiency therapy?
If you have CVI, The Vein Center Doctor suggests taking these steps to help get Medicare coverage for your necessary treatment.
- Get an evaluation from a vein specialist to diagnose your condition and determine appropriate therapies.
- Ask your doctor to provide documentation that shows medical necessity for the recommended treatments.
- Submit any required paperwork for prior authorization if needed for certain procedures or prescription meds. You may need to contact your Medicare Administrative Contractor (MAC) for more information and confirmation.
- Enroll in Medicare Part A and B to get coverage for inpatient and outpatient vein care.
- Sign up for Part D if you need prescription drug coverage for CVI medications.
- Compare Medicare Advantage plans (Part C) in your area to find one that suits your needs.
- Work with an insurance agent to select supplemental coverage like a Medigap plan.
- Find in-network vein specialists, hospitals, and providers to lower your treatment costs.
- Keep records and follow up on all claims to ensure proper processing and payment.
- Appeal any denied claims and cite supporting clinical evidence for coverage. If a claim is denied, you have the right to appeal the decision.
Tired of CVI Symptoms? We Can Help!

Medicare provides coverage for medically necessary treatment of chronic venous insufficiency to help alleviate your symptoms and improve vein health in your legs. Following proper treatment guidelines, utilizing Medicare-approved therapies, and collaborating closely with your doctors can help ensure you get the appropriate care and coverage.
Consider scheduling a consultation with The Vein Center Doctor – our vascular experts can diagnose the cause of your CVI and craft an effective treatment plan tailored to your specific needs while optimizing your Medicare benefits.