Chronic venous insufficiency (CVI) is a vascular condition that occurs when one-way vein valves of the lower extremities fail to control reflux or backward blood flow. CVI often leads to varicose veins, which affects around 60 million adults in the United States. The management of this underdiagnosed vein disease accounts for around 2% of the nation’s total healthcare.
So what are the best treatment methods for chronic venous insufficiency? Conservative therapy methods such as exercises for the legs, and pharmacological prescriptions are among the least invasive treatments for alleviating the most common symptoms of CVI. For more severe cases, surgical procedures are employed. Outpatient treatments such as sclerotherapy, radiofrequency ablation, and VenaSeal are also among the possible treatments.
Causes of Chronic Venous Insufficiency
CVI, albeit being a prevalent cardiovascular disease, was once heavily understudied in the field. In 1994, an international consensus created the CEAP, a comprehensive classification tool aiming to communicate a uniform approach to diagnosis, treatment, and etiology of the disease in the medical community. It stands for the clinical (C), etiological (E), anatomical (A) and pathophysiological (P) classifications of CVI.
According to CEAP’s etiological categories, the causes of CVI can be classified as follows:
1) Primary chronic venous insufficiency
Primary chronic venous insufficiency refers to the intrinsic manifestation of symptoms without a prior precipitating event. Its causes are uncertain, but it is commonly attributed to genetic defects or environmental factors changing venous wall biochemistry. CVI under primary etiological classification accounts for around 70% of the disease’s occurrence.
Primary CVI is associated with increased extracellular matrix remodeling, lower venous elastin content, and presence of inflammatory infiltrate.These factors contribute to further vein dilation and more incompetent vein valves, giving rise to its common symptoms. These factors can also exacerbate the occurrence of deep vein thrombosis.
2) Secondary chronic venous insufficiency
Whereas primary CVI is inherent and idiopathic, secondary CVI is caused by a precipitating medical condition – the most common of which is deep vein thrombosis (DVT). Deep vein thrombosis is best explained as an increased occurrence of blood clot within the deep veins. CVI caused by DVT is also called “post thrombotic syndrome”
Secondary CVI can also be caused by external factors, including vascular trauma from blunt or penetrative damage to the veins.
3) Congenital chronic venous insufficiency
Congenital CVI refers to chronic venous disease caused by inborn genetic mutations precipitating cardiovascular abnormalities. The most common example of this is the Klippel-Trenaunay syndrome which is characterized by softened tissue, venous ulcer development, DVT, venous hypertension, and bone hypertrophy.
CVI is also associated with risk factors from environmental and lifestyle influences such as:
- Lack of exercise and inactivity
- Prolonged sitting or standing
- Aging
- Female sex
- Obesity
- Family medical records of CVI, varicose veins, or other cardiovascular diseases
Symptoms of Chronic Venous Insufficiency
Chronic venous insufficiency symptoms progress slowly, and don’t immediately manifest, making it difficult to diagnose. To prevent more severe cases of CVI, below are some of the most common symptoms you should watch out for, especially in your lower extremities and the leg area:
- Vein dilation (e.g., varicose vein, spider vein)
- Increased venous pressure
- Edema on the legs
- Itching skin on the legs
- Lower leg ulcers
- “Pins and needles” sensation in the legs
- Hyperpigmentation (darkening of the skin)
- “Leathery” looking skin
Conservative Therapy
Chronic venous insufficiency treatment involves a preliminary method employing conservative methods. These are non-invasive steps in alleviating the symptoms of CVI and preventing its progression in a more severe case.
1) Exercise
A structured and graded exercise therapy is also administered to patients with chronic venous disease. In a 2004 study, it was evident that a 6-month program of structured exercises targeting physical conditioning of calf muscles has improved calf muscle and leg vein pumping function. Despite not showing significant changes on venous reflux, a structured exercise program is still a beneficial supplement to medical treatments for patients with advanced CVI.
2) Medications
The use of venoactive drugs in relieving CVI pain and swelling and hastening the healing of venous ulceration is best combined with compression therapy. Venoactive drugs possess properties that strengthen venous tone, control platelet coagulation, and improve capillary permeability, and stabilize inflammatory response. These substances include flavonoids (γ-benzopyrenes), coumarins (α-benzopyrenes), and saponosides (horse chestnut extracts).
Other drugs such as pentoxifylline and sulodexide have been tried and proven to improve the healing rates of venous ulceration and improve inflammatory response.
3) Wound and Skincare
To preserve skin integrity, it is also necessary to prevent infection and provide consistent skin care treatments. Topical moisturizers, for instance, are recommended to alleviate dry skin and reduce skin fissuring. Topical steroids, meanwhile, can assist in treating stasis dermatitis. Hydrocolloids and foam dressings are also applied to help accelerate the healing of venous stasis ulcers.
Surgical Treatments
For severe cases and patients with nonresponsive symptoms to conservative management therapy, vascular surgery is employed to prevent further complications that may develop into more advanced CVI. Below are some of the most effective surgical procedures used to treat severe CVI:
1) Ligation and Stripping
Vein ligation or tying off of the problematic leg vein is performed to prevent the pooling of blood.. It’s often accompanied by stripping, which involves the surgical removal of a severely damaged vein through small incisions. Venous ligation and stripping are found to be effective in improving blood flow, accelerating ulcer healing, and alleviating CVI symptoms.
These methods are often used for truncal veins and vein tributaries, wherein backward blood flow and varicose veins are targeted through interruption and removal.
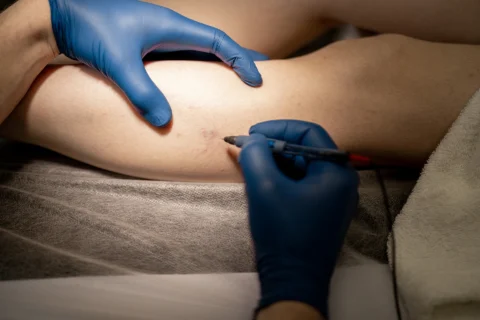
2) Ambulatory Phlebectomy
Ambulatory phlebectomy involves the use of phlebectomy hooks to perform needle punctures through the skin to excise the damaged blood vessel. It mainly targets varicose veins near the skin’s surface.
3) Vein Bypass Surgery
For severe cases in the femoral vein, a vein bypass surgery is another option. This is performed by extracting a portion of a healthy vein in another part of the body and using it to reroute blood into the affected area.
Excellent Vein Treatments from Vein Center Doctor

Surgical procedures often pose great risks and involve longer downtime, while conservative management requires intensive and religious maintenance. Here at Vein Center Doctor, we value our patients by offering top-of-the-line technology in cardiovascular outpatient treatments.
Combined with our team’s healthcare expertise, we offer the best non-invasive outpatient vein treatment options such as sclerotherapy, radiofrequency ablation, compression therapy, and VenaSeal.
1) Compression Therapy
Compression therapy is the standard treatment for chronic venous insufficiency, and is often combined with other minimally-invasive procedures for maximum results. Compression therapy is a fully non-invasive therapy utilizing compression garments such as graded elastic compression stockings and layered bandaging to control fluid retention resulting from venous hypertension. Its benefits include:
- Acceleration of ulcer healing
- Alleviating leg pain and swelling
- Normalizing skin pigmentation
- Reduction of venous reflux
2) Sclerotherapy
Venous sclerotherapy employs the injection of sclerosing agents into the affected vein as treatments for varicose vein, spider vein, vascular malformation, and superficial vein reflux. Sclerosing agents such as 23.4% sodium chloride and sodium iodide induces dehydration of vein endothelial cells which in turn collapses the affected vein and stimulates redirection of blood into healthier veins.
Sclerotherapy side effects include hyperpigmentation, local inflammation, and vein swelling. Of the two kinds of sclerotherapy, ultrasound-guided foam sclerotherapy is more effective than liquid sclerotherapy due to blood dilution differences between the delivered sclerosants.
3) Radiofrequency Ablation
Radiofrequency ablation is a minimally-invasive procedure that uses thermal energy delivered through radiofrequency catheter to destroy the inner vein wall, closing the vessel and redirects blood in the legs to healthy veins. It’s a safe and FDA-approved procedure, requiring only local anesthesia. A 2002 trial of the procedure reported significant improvement in the quality of life of patients, with 95% reported satisfaction.
This procedure is performed with the patient lying supine. Prior to the procedure, the affected leg will be sterilized, then the catheter will be inserted to the affected vein in the legs. This procedure is done in combination with the use of compression stockings to avoid bruising, after which the patient is able to return to normal routine.
4) Endovenous Laser Treatment
Endovenous laser ablation, like radiofrequency ablation, also uses thermal energy to target the affected veins to prevent backward blood flow and pooling of blood. Except, instead of a radiofrequency catheter, laser ablation uses a catheter with laser fibers of either 810-nm or 940-nm diode to destroy the vein wall, forming a scar tissue and redistributing blood to healthy veins.
5) VenaSeal
VenaSeal is a new innovation in minimally invasive vein treatment procedures. VenaSeal is an adhesive administered using a catheter to close off the diseased vein. It involves an initial ultrasound examination to locate the affected veins at the distal point through which the catheter will be inserted.
A saline solution will be administered prior to the sealing to flush out a blood clot, then 3cm of the VenaSeal adhesive will be injected every 3 seconds until the entirety of the target vein is sealed. As with most of the treatments, a compression bandage will be placed over the treatment area.
Professional Outpatient Vein Treatments at Vein Center Doctor
For the longest time, chronic venous insufficiency has been an enigmatic vein disease affecting many individuals until the development of innovative techniques and technology. Through proper conservative treatments and non-invasive procedures, our vein clinic assures that you need not worry about greater consequences.
Vein Center Doctor is dedicated to providing professional and patient-centered care to our valued patients. Headed by Dr. Rahul Sood, our team of healthcare experts are always at your service. Start your journey to better vein health by booking an appointment with us at 862-227-1143 (NJ) or 862-227-1054 (NY) for your free consultation.