Chronic venous insufficiency happens when a damaged leg vein fails to function properly. It leads to the appearance of unwanted veins, but it may also result in more serious venous disease if left untreated. There are a few chronic venous insufficiency treatment options available, but combining vein and dermatology treatments is one of the best treatment plans for most patients.
So how exactly does combining vein and dermatology treatment help manage chronic venous insufficiency? Vein treatments for CVI ensure that the condition is treated in its roots while dermatology treatments are for erasing the symptoms of CVI on the surface of the skin, such as spider veins, reticular veins, varicose veins, and more. When performed together, these treatments lead to better results that make the veins function better.
Managing Chronic Venous Insufficiency With Dermatology Treatments
Chronic venous insufficiency (CVI) or venous reflux is a type of chronic venous disease caused by damage in the veins of the lower legs. It’s a common vein disease that affects about 2.5 million Americans, about 20% of whom even develop venous ulcers after a while.
Unwanted leg veins are one of the symptoms of chronic venous insufficiency so many patients turn to dermatology treatments to reduce their appearance. While this may be effective for some, vein treatment should still be performed to treat the underlying medical condition properly.
What Chronic Venous Insufficiency Is
When a patient has chronic venous insufficiency, their blood can’t flow well and return to the heart, causing it to pool inside the affected vein. CVI may happen to any blood vessel in the legs, including the deep vein, superficial vein, and perforating vein. Improper blood flow and pooling inside the diseased vein means that there’s also a higher blood pressure inside.
What Causes It
Any vein problem that causes increased blood pressure and poor circulation inside the lower leg vein can also cause the blood vessel there to dilate. This damages the valves and affects the function of the vein, leading to chronic vein disease. Here are some of the most common reasons why there’s an increase in the blood pressure inside the veins:
- Congenital leg vein malformation – Some people are born with malformations in their leg veins, like the lack of valves. This affects blood circulation and venous pressure in the area, which may lead to CVI and other venous disorders.
- Blood clots inside the vein – A blood clot inside the vein blocks the blood flow, which causes pressure buildup. This leads to permanent damage to the blood vessel (or their valves) that still persist even after the clot is dislodged.
- Leg surgery or injury – Any surgical procedure performed on the patient’s leg may block the flow of blood through the veins, resulting in chronic venous insufficiency or venous hypertension.
- Weight gain or pregnancy – The added weight of obesity or pregnancy increases pressure inside the veins of the lower legs. This results in damage to veins or valves.
- Standing or sitting for long periods – The muscles in the legs are important in blood circulation so standing or sitting for long periods without much movement decreases blood flow from the legs to the heart. This leads to an increase in venous pressure and blood pooling.
What the Symptoms Are
The early stages of chronic venous insufficiency may be difficult to detect because some patients might not see or feel symptoms – just the occasional ache and heaviness in their legs. But if left untreated, the chronic venous insufficiency symptoms may become more noticeable until they start interfering with the patient’s daily activities and quality of life. Here are some of the milder and more common signs and symptoms of CVI:
- Tired or achy legs
- Leg cramping at the end of the day or night
- Heavy or full feeling in the legs
- Tingling or burning sensation in the legs
When the CVI starts becoming more serious, patients might start noticing more severe symptoms like:
- Swelling – Persistent chronic venous insufficiency causes edema or swelling in the lower legs and ankles. In some cases, patients only notice the swelling at the end of the day, while others observe it at all times. Swelling might be less prominent in the morning since keeping the legs elevated at night helps relieve edema.
- Dilated veins – Vein dilation is one of the most common symptoms of CVI. They usually appear as thin blue or purple flares near the surface of the skin (spider vein) or wider, twisted veins that bulge on the surface (varicose vein).
- Skin changes – Long-term blood pooling and venous hypertension causes the skin in the legs to become more reddish-brown or tan than the rest of the skin. This skin discoloration is usually noticeable around the ankle at first, but it may also spread to the shins and feet. Aside from discoloration, other changes may also occur like dryness, scaling, scabbing, and open sores from scratching.
- Venous ulceration – Open and non-healings sores caused by CVI are known as venous ulcers or venous stasis ulcers. They’re usually found on the inner ankle, but they may also develop on the shin and outer ankle area. A venous ulcer may be a result of repeated scratching, trauma, or injury. It may also start as a small sore but worsen into a bigger venous leg ulcer.
What the Stages Are
Venous disorders like chronic venous insufficiency and venous reflux can be classified into 7 stages. Each stage is characterized by different clinical signs that a healthcare provider observes when they examine the patient’s legs. Here are the different stages of venous disorders and how they look:
- Stage 0: Patients might not see or feel symptoms, except for the occasional achy or tired legs.
- Stage 1: There are some visible blood vessels just below the surface of the skin, like spider veins and reticular veins.
- Stage 2: There are bulging varicose veins below the skin that are at least 3 mm wide.
- Stage 3: The ankles or lower legs are swelling, but there are no other skin discoloration or changes yet.
- Stage 4: There are some changes in the color or texture of the skin in the ankles and legs.
- Stage 5: There are some ulcers, but they heal after some time.
- Stage 6: Patients have active venous ulcers that won’t seem to heal.
Chronic venous insufficiency is only diagnosed if the patient has at least stage 3 symptoms. This means having spider veins and varicose veins don’t necessarily mean an individual has CVI.
However, these unwanted leg veins are signs of blood flow problems that might worsen over time and become CVI. Always make sure to tell the healthcare provider if there are any other signs of venous disorders on the skin.
Why Chronic Venous Insufficiency Should Be Treated
When CVI and other venous diseases are left untreated, they may raise the vein pressure in the affected area until the capillaries burst. This gives the skin a reddish-brown discoloration and makes it easier to break if scratched or bumped. Burst capillaries can also cause venous stasis ulcers and stasis dermatitis that easily become infected, spreading to nearby tissues.
Aside from changes on the skin, CVI can also cause severe pain and discomfort that affects the patient’s quality of life. In some severe cases, patients may develop other venous conditions like deep vein thrombosis, pulmonary embolism, severe venous ulceration, and more.
The good news is that chronic venous insufficiency is manageable even without vascular surgery. There are lots of vein and dermatology treatments that patients can choose from after consulting with a healthcare provider about their vein condition.
How Dermatology Treatments Help With CVI

The appearance of unwanted leg veins like varicose veins and spider veins is one of the common symptoms of chronic venous insufficiency. Since many patients find them unpleasant to look at, they turn to dermatologists to help get rid of the pesky leg veins. To eliminate the visible veins on the skin, here are some dermatology treatments that skin experts use:
1) Laser Treatments
Laser treatments have a lot of medical and dermatological applications. In the case of CVI patients, they use laser treatments to get rid of the pesky veins that appear near the surface of the skin. This dermatology treatment works best for smaller veins like spider veins, reticular veins, and tiny varicose veins.
During the laser treatment, the doctor uses a laser device to deliver focused light that causes the unwanted vein to clot, dry, and close. Laser treatments are less invasive than closure systems and other venous treatments because they don’t involve incisions or injections.
2) IPL Therapy
Intense pulsed light (IPL) therapy for pesky spider veins works similarly to laser treatments – it uses a high-intensity light source to heat and damages the vein wall of the diseased vein. This dermatology treatment eventually causes the damaged vein to collapse and disappear over time.
IPL treatments only affect the deeper layers of the skin so patients don’t have to worry about scarring or burning the top layers of the skin. The treated veins are eventually reabsorbed by the body over the next few weeks until they’re gone and faded.
3) Retinoids
Retinol creams are typically used by skincare patients to eliminate a wide variety of skin conditions, including unwanted veins. They’re made of tretinoin and retinol which thicken the skin, causing the spider veins to look less visible.
Although retinol products can help improve the appearance of the skin, patients must remember that this kind of treatment doesn’t directly eliminate or treat spider veins – they only improve the skin’s health and condition so spider veins don’t look as noticeable as usual. Patients are also required to take these products regularly for a few months before they experience the results they want.
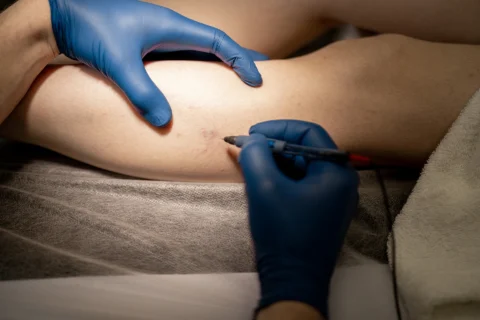
4) Sclerotherapy
Sclerotherapy is considered a venous treatment for unwanted veins, but a lot of dermatologists also perform this procedure for clients who want to erase spider veins and varicose veins for aesthetic purposes. They can perform this treatment as long as they have the medical education required to properly do it.
During sclerotherapy, the doctor injects a sclerosant into the affected vein. The chemical contains a high concentration of saline or detergent that irritates and scars the problem vein. This causes the vein wall to collapse and disappear within 3 to 6 weeks after the appointment.
4 Veins Treatments to Combine With Dermatology Treatments for CVI
Dermatology treatments are mostly concerned with erasing the visible veins on the skin, so some of them don’t directly address the root of chronic venous insufficiency. On the other hand, having venous treatments alone might not be enough to restore the original, healthy appearance of the skin. Combining both types of treatment can give patients the kind of results they want for their skin while helping them manage their CVI.
At Vein Center Doctor, we recommend the following vein treatments to combine with dermatology procedures for the best CVI management plan:
1) RFA for Varicose Veins
Radiofrequency ablation (RFA) is a type of varicose vein treatment that uses electricity to heat the damaged veins, causing them to collapse and seal off. It’s usually accompanied by Duplex Ultrasound to ensure that the right vein is treated.
During RFA treatment, the leg is injected with local anesthesia. The vein is punctured with a small needle where a catheter is inserted. The catheter delivers heat inside the vein until it’s closed off.
2) Sclerotherapy
Sclerotherapy at Vein Center Doctor is similar to how sclerotherapy is performed in other vein centers: a sclerosing agent is injected into the damaged vein to scar and seal it off. The blood is then redirected into nearby healthier veins. The treated vein is eventually reabsorbed by the nearby tissues.
3) VenaSeal
VenaSeal is another non-surgical treatment for varicose veins. It uses an FDA-approved medical glue to close the damaged vein, causing blood to flow to other veins near the treatment area. Since the treatment is minimally invasive, patients only experience minimal discomfort during the procedure. They may even work and return home on the same day as their appointment.
4) Compression Therapy
Compression therapy is one of the more traditional yet highly effective treatments for chronic venous insufficiency. It involves using compression stockings or socks to improve blood flow in the legs and lower extremities. It can also be combined with other treatments like sclerotherapy, RFA, and VenaSeal to speed up healing and prevent CVI’s progression to venous thrombosis.
Eliminate Pesky Leg Veins With Vein Center Doctor

In some cases, unwanted leg veins are more than just a cosmetic concern. They might be a symptom of a more serious vein condition like chronic venous insufficiency, which may require both dermatology and vein treatments.
Before your chronic venous insufficiency worsens and starts affecting your quality of life, consult with our experts at Vein Center Doctor today for the best vein solutions. Call us today to book your first appointment and discuss a CVI treatment plan for you.