Feeling the pain of heavy, achy legs that swell throughout the day? You may have chronic venous insufficiency (CVI). While symptoms may persist, today’s treatments provide new hope.
Look beyond temporary pain relief – properly treat the root cause. From compression stockings to minimally invasive procedures, options exist to improve circulation and quality of life.
At The Vein Center Doctor, we stay on top of the most advanced CVI therapies. Read on as we detail progressive treatment approaches tailored to your needs – and get ready to put the spring back in your step.
What is chronic venous insufficiency, and how is it treated?
Chronic venous insufficiency (CVI) is a condition in which the veins in the legs are unable to efficiently transport blood back up to the heart. As described in a 2017 article by the Journal of Clinical Medicine, Maedica, this is typically caused by faulty valves inside the veins that prevent blood from flowing backward.
Blood ends up pooling in the lower extremities, leading to a variety of symptoms. At The Vein Center Doctor, we treat CVI using a combination of compression stockings, medications, minimally invasive procedures, and lifestyle changes aimed at improving circulation and reducing symptoms.
Some of our primary treatment methods include graduated compression socks to help blood flow, diuretics to reduce swelling, procedures like endovenous laser ablation to collapse damaged veins, and recommending exercise and leg elevation to our patients. While CVI cannot be cured, diligent treatment can significantly improve quality of life.
What are the symptoms and signs of chronic venous insufficiency?
- Achy, tired, heavy feeling legs – As Hopkins Medicine explains, this achiness and fatigue often get worse over the course of the day and after prolonged standing or sitting. It’s from the accumulating blood that isn’t circulating properly.
- Leg swelling – StatPearls mentions that the pooling of blood and ineffective calf muscle pumping can lead to edema and swelling of the lower legs and ankles. This often worsens in warm weather.
- Visible varicose veins and spider veins – The high venous pressure causes veins to abnormally bulge under the skin. Existing varicose veins tend to worsen.
- Skin discoloration – Reddish-blue skin discoloration can appear, typically around the ankles.
- Itching and dermatitis – The inflamed skin around the ankle area often becomes extremely dry and itchy.
- Leg ulcers – In severe advanced CVI cases, the pressure and poor circulation result in skin ulcerations usually near the medial ankles.
How is chronic venous insufficiency diagnosed and treated, including surgical options?
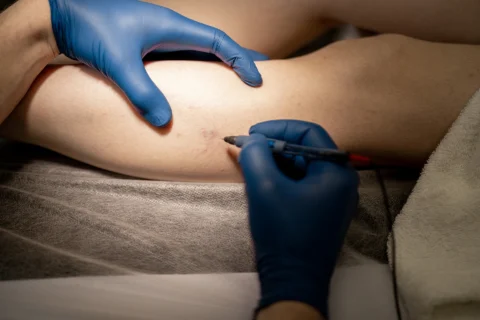
Our diagnostic process at The Vein Center Doctor begins with a medical history and physical exam to assess symptoms and check for signs of CVI. We then utilize ultrasound imaging to evaluate blood flow in the veins and identify any faulty valves or blockages. Additional tests like venous plethysmography can also measure venous pressure.
Once diagnosed, we first recommend conservative treatments like graduated compression stockings and medications like diuretics or anticoagulants. If symptoms persist, we consider minimally invasive procedures like endovenous laser ablation, radiofrequency ablation or sclerotherapy to collapse damaged veins.
In rare, severe cases where conservative treatments fail, we may recommend surgery such as vein ligation or valve repair. However, our goal is always to take the least invasive approach possible that will provide lasting relief to our patients.
Is chronic venous insufficiency a dangerous condition?
While not immediately life-threatening in most cases, chronic venous insufficiency can greatly impact patients’ quality of life when left untreated. Per our experience, severe CVI cases can lead to major skin ulcerations, cellulitis infections, bleeding episodes, and recurrent thrombophlebitis.
Patients with CVI are also at increased risk for developing deep vein thrombosis. While the condition itself is not fatal, it also cannot be cured completely. However, with consistent proper treatment and lifestyle adjustments, patients can often achieve stable improvement in their symptoms and vascular health.
What are the care plans for chronic venous insufficiency?

At The Vein Center Doctor, we grade CVI as mild, moderate, or severe based on the extent of symptoms and the presence of complications. Mild CVI produces minimal swelling and aches that can be managed with compression stockings and exercise.
Our care plans are tailored to each patient’s severity level. We educate patients on medications, compression wear use, staying active, wound care if needed, and follow-up with us for continued monitoring and treatment adjustments.
For example, a study by the National Institute for Health and Care Excellence provides guidelines on antimicrobial prescribing for leg ulcer infections, which include the use of IV antibiotics for more severe infections.
Can chronic venous insufficiency be reversed or cured?
While there is currently no definitive cure for chronic venous insufficiency, the condition can often be effectively managed with diligent treatment based on our experience. The vein valve damage and dysfunction that causes CVI is a progressive, irreversible process.
However, optimizing venous circulation and blood flow with the appropriate therapies can help stabilize or slightly improve some patients’ conditions over time.
Symptoms are controlled best with a combination treatment approach of medications, compression garments, minimally invasive procedures, exercise, weight management, and leg elevation. The treatment plan must be maintained long-term as well to prevent recurrence of symptoms.
The core treatments we recommend include:
Compression Stockings
- First-line treatment to improve circulation
- Graduated compression socks/sleeves
- Optimal compression level based on severity
- Proper fitting and usage instructions provided
- Worn daily for significant symptom improvement
Medications
- Diuretics reduce leg swelling and venous pressure
- Anticoagulants prevent worsened circulation
- Antibiotics treat leg ulcer infections
- Minimally Invasive Procedures
- Endovenous laser ablation
- Radiofrequency ablation
Sclerotherapy
- Collapse damaged veins causing symptoms
- Outpatient with minimal downtime
Lifestyle Optimization
- Calf exercise aids circulation
- Leg elevation utilizes gravity
- Weight management reduces vein pressure
- Smoking cessation improves vascular health
- Movement breaks avoid prolonged sitting/standing
Are there new and innovative treatments for chronic venous insufficiency?
Some emerging treatments showing promise in studies include experimental drug therapies like vasoactive medications to improve circulation and growth factor injections to heal ulcers, newer minimally invasive procedures like mechanochemical ablation, external counterpulsation devices to enhance venous return, and early research on bioengineered vein valves and stem cell injections to repair damaged veins.
- For example, a narrative review discusses the use of a vasoactive drug called Micronized Purified Flavonoid Fraction (MPFF) to relieve CVI symptoms and improve patient quality of life.
- A meta-analysis also found that growth factors significantly increased chronic wound healing.
- A study on mechanochemical ablation showed a 95.6% technical success rate and 87.3% clinical improvement rate.
While still experimental, these innovations may offer less invasive future options for symptom relief. We carefully evaluate all new technologies before usage.
What is the relationship between chronic venous insufficiency and constipation?
From our experience, there is no direct relationship between CVI and constipation. However, a study published on PubMed found that conditions increasing intra-abdominal pressure, like constipation, can trigger both lower extremity CVI and hemorrhoids.
Straining with bowel movements can also temporarily worsen CVI pressure and swelling. Additionally, some CVI medications like diuretics may contribute to constipation as a side effect, according to research from the German ESTHER cohort.
That’s why we advise patients to maintain regular soft bowel movements through a high-fiber diet and active lifestyle, based on evidence from Healthline. Proper hydration, exercise, and avoiding excessive straining can minimize CVI symptom aggravation.
What are the emergency and medical treatments for chronic venous insufficiency?
In urgent situations like a leg ulcer infection or bleeding varicose vein, we advise seeking emergency care right away. Hospitalization may be required for issues like excessive blood loss, cellulitis, or extensive ulceration.
Vital medical treatments can include IV antibiotics to treat infection, debridement of necrotic tissue, multi-layer compression bandages, pain medication, leg elevation, and strict bed rest. If an underlying blood clot led to severe symptoms, anticoagulants would be administered.
Following discharge, we provide instructions on medications, compression stockings, wound care and activity modification to stabilize symptoms long-term.
Are there natural ways to treat chronic venous insufficiency?
Some integrative therapies may provide temporary CVI relief when used cautiously with medical treatments, but are not proven cures currently.
A 2012 Cochrane review of 17 RCTs found that oral horse chestnut seed extract appeared to improve CVI signs and symptoms compared to a placebo, though larger, definitive RCTs are still needed.
Some other naturopathic options:
- Yoga/meditation for swelling/pain reduction
- Contrast baths to stimulate circulation
- Massage towards heart by a trained therapist
- Herbs under medical supervision
The Vein Center Doctor focuses on traditional, conservative evidence-based therapies performed by vein experts as the primary approach to optimal CVI management.
Can exercise help manage chronic venous insufficiency?
Yes, certain lower body exercises can significantly help manage chronic venous insufficiency symptoms. At The Vein Center Doctor, we specifically recommend:
- Low-impact cardio like walking, swimming, and cycling to engage the calf muscle pump and improve overall circulation without added strain.
- Calf raises, toe lifts, leg extensions, and hamstring curls to strengthen calf and leg muscles involved in effective venous return.
- Yoga poses like legs on the wall inversion that can aid circulation when held for several minutes.
- Avoiding weightlifting, sprinting, jumping, or other strenuous activities that may increase venous pressure.
- Checking with us to establish safe exercise limits and gradually increase duration and resistance.
- Using well-fitted, medical-grade compression stockings during workouts.
- Staying hydrated and taking breaks as needed.
According to a 2016 systematic review, current evidence on the efficacy of physical exercise for CVI is limited. However, light, low-impact exercise shows promise for engaging the calf muscle pump to improve circulation.
Is walking beneficial for those with chronic venous insufficiency?
Yes, walking is an excellent low-impact exercise for managing chronic venous insufficiency based on our experience. The calf muscle pump is activated during walking, which can aid venous return, as discussed in a study on PubMed.
We suggest starting with short, slow walks. Gradually increase distance as tolerated, use compression stockings, and take rest breaks. Monitor for skin irritation and avoid walking if blisters/abrasions develop. Check with your vein specialist about appropriate walking targets and intensity.
Does massage offer benefits for individuals with chronic venous insufficiency?
According to our observations, gentle massage by a properly trained therapist can temporarily reduce leg edema and heaviness in CVI patients. A study found massage increased venous blood flow in the legs.
However, effects are temporary and direct pressure over varicose veins should be avoided. Overall, massage is not a cure but may be a beneficial addition when used cautiously alongside medical treatments.
Who is the appropriate doctor to treat chronic venous insufficiency?
We recommend seeking out a board-certified vein specialist or phlebologist for optimal CVI treatment. Vascular surgeons are also well-trained in this area. Some other providers may oversee CVI care and provide referrals.
What’s important is to look for a physician extensively familiar with chronic venous insufficiency diagnosis and management. Our team has specialized expertise and provides complete CVI treatment.
You Deserve Healthy Legs – Our Team Is Ready to Get You on the Road to Recovery

Chronic venous insufficiency can greatly impact quality of life but implementing an appropriate, comprehensive treatment plan can significantly improve symptoms.
Partnering with a dedicated vein care specialist allows access to the latest minimally invasive procedures, prescription medications, compression garments, lifestyle changes, and ongoing monitoring to successfully manage CVI long-term.
Contact our office to learn about cutting-edge therapies that can help put you back on the path to healthy veins and legs.