Are spider veins just a cosmetic issue or could they be a sign of something more serious?
While most small spider veins and reticular veins are typically just a cosmetic concern caused by telangiectasia or venous stasis within the superficial venous system, it's important to see your doctor to rule out any underlying vascular disease or venous insufficiency that could be causing them.
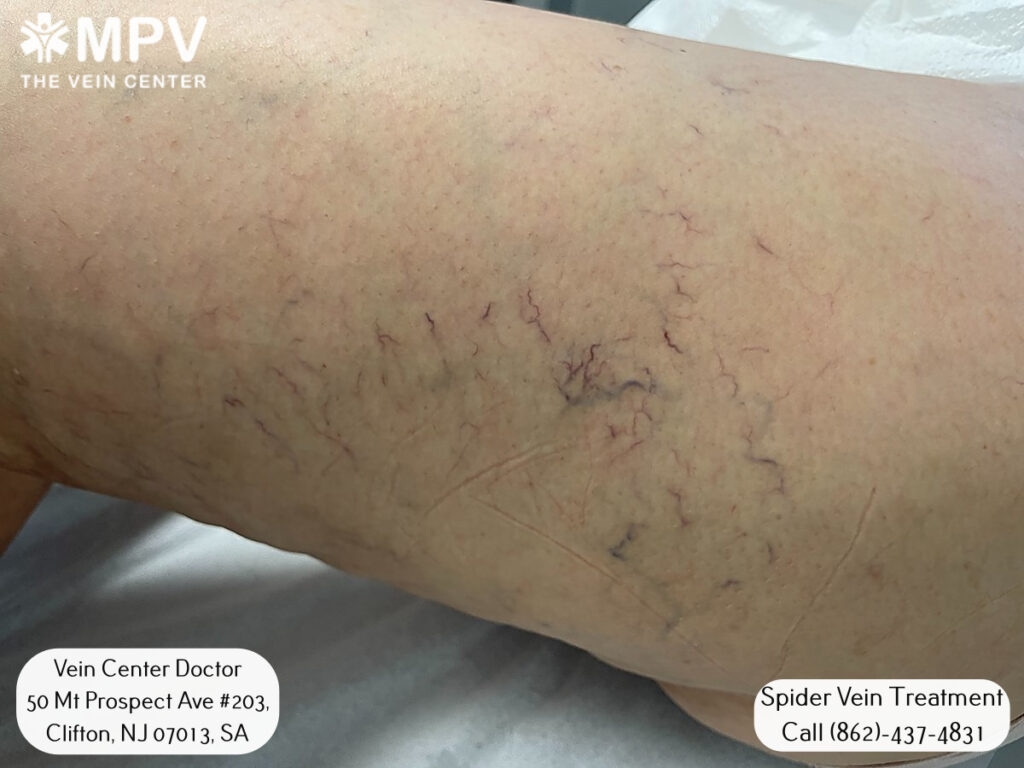
Larger varicose veins or clusters of spider veins that appear quickly may signal a deeper issue like venous hypertension, venous reflux disease, or a history of deep vein thrombosis that has led to venous valve incompetence.
Seeking medical guidance is wise to check for venous reflux, venous malformations, or the potential for developing venous edema, venous stasis dermatitis, or even serious problems like venous ulcers if left untreated. Especially in those with a family history of venous thrombosis or superficial venous thrombosis who are at higher risk for deep problems.
Early detection by a medical professional can help prevent worsening venous disorders and ensure proper venous thrombosis prophylaxis if needed. While most of the time spider veins are a minor cosmetic issue, it's always best to have a doctor examine any new or rapidly spreading vein issues to check for more serious underlying venous disease.
Living with unwanted veins is a thing of the past, when you can simply schedule a free consultation with Vein Center Doctor and find your ideal solution today.
It's generally best to see a medical professional if spider veins or small reticular veins begin appearing and seem to be worsening at a rapid pace.
New or progressively enlarging veins could potentially signal an underlying issue like venous reflux disease, venous valve incompetence, or chronic venous insufficiency that is leading to increased venous hypertension and venous stasis within the leg veins. This is especially true if symptoms also develop such as aching, heaviness, swelling (venous edema), or skin changes around the veins like hyperpigmentation or redness indicative of venous stasis dermatitis.
Seeking prompt medical care is advised if one has a family history putting them at higher risk for venous thrombosis, either superficial venous thrombosis or deep vein thrombosis. It's also important to see a doctor for evaluation if spider veins or surrounding skin ulcerations like venous leg ulcers do not improve with elevation and compression treatment.
This could point to a need for further vascular testing to rule out other issues impacting venous outflow and potentially leading to problems such as recurrent leg ulcers if left unaddressed.
Overall, seeing a physician is warranted if spider veins are rapidly expanding or accompanied by pain, tenderness, tissue damage, or signs of poor healing - as this combination could suggest an underlying pathology contributing to venous reflux or venous stasis within the leg that requires medical management and treatment to prevent long-term complications like non-healing venous ulcers or worsening chronic venous insufficiency. Early evaluation is advised when potential risk factors or warning signs are present.
While very small, finest spider veins or reticular veins may regress or fade somewhat over time on their own as part of the natural aging process, larger visible spider veins rarely resolve spontaneously without treatment. This is because as we age, gravity and repetitive muscle contractions take a toll on the venous vascular system.
Conditions like venous malformations, previous venous thrombotic events, or thromboses like deep vein thrombosis that have damaged venous valves increase one's risk of developing problematic venous reflux conditions that support persistent spider vein formation over the long-term.
For some individuals, simple lifestyle changes involving regular exercise, weight management, and compression stockings can help smaller spider veins from worsening dramatically. But sizable, bulging spider veins are typically not reversible without sclerotherapy, laser treatment, or advanced ablation modalities to treat underlying venous reflux or properly occlude the affected veins.
This is due to the prolonged effects of venous hypertension and chronic venous stasis at a deeper level in cases where faulty venous drainage cannot self-correct. In such instances, medical intervention offers the best potential for meaningful and long-lasting spider vein improvement when conservative measures prove inadequate. While small superficial telangiectasias may fade, large spider veins generally require treatment to properly resolve once they develop without intervention.
There are several factors that can increase one's vulnerability to developing problematic spider veins or experiencing venous insufficiency issues like chronic venous insufficiency over time.
Genetics certainly plays a role, as having a family history of varicose veins or venous ulcers indicates a heritable predisposition. Increasing age is also a common factor, as the venous architecture suffers progressive damage with each passing decade. Pregnancy notably increases risk due to the effects of hormonal changes and blood volume overload on fragile veins.
Carrying excess weight, especially abdominal obesity, creates hydraulic pressure that challenges venous efficiency. Occupations involving extensive time spent standing without breaks similarly stress the circulatory system. Past trauma such as lower extremity injuries increasing the likelihood of developing venous malformations or a prior deep vein thrombosis event that results in venous valve incompetence also heighten spider vein probabilities.
Developing chronic venous insufficiency through multiple high-risk variables makes one more prone to the telangiectasias and reticular growths that constitute spider veins. Maintaining a lean physique, exercising regularly, elevating legs when possible, and considering compression garments for those at higher inherent risk can help compensate for vulnerability and potentially deter spider vein formation over the long term.
Maintaining a healthy weight and regular exercise can help prevent worsening of spider veins. Staying hydrated, elevating legs, and wearing compression stockings may also provide relief.
It's generally best to wait until after pregnancy or significant weight changes to have spider veins treated, as new ones could form or existing ones worsen.

Options may include sclerotherapy, laser or light treatments, ultrasound or radiofrequency ablation, and in some cases surgery to remove larger veins.
Non-invasive treatments like sclerotherapy or lasers often require just a single treatment, while more advanced cases may need multiple sessions spaced 4-6 weeks apart.
With proper treatment and skin care, most people can expect a year or more before retreatment is needed. Maintaining a healthy lifestyle can help prevent new spider veins from developing.
Find exactly what you need to get rid of your vein-related problems. Dr. Sood and the rest of our team at Vein Center Doctor are ready to help: schedule your free consultation today.
Most Insurance is accepted for treatment