As many as 4 in 10 people in the United States have chronic venous insufficiency. This relatively high burden of disease necessitates effective treatments that must be employed to improve the quality of life of these people suffering from the disease.
So can chronic venous insufficiency be corrected by using compression therapy? Compression therapy can’t correct chronic venous insufficiency. What it does though is help manage the symptoms associated with this venous disease and prevent its progression to other complications such as venous ulceration.
Compression Therapy As The Standard Of Care For Chronic Venous Insufficiency
Chronic venous insufficiency is characterized by the pooling of blood in the deep vein. It’s a multifactorial disease brought by the family history of cardiovascular risk factors and a previous medical history of deep vein thrombosis that raises the clinical suspicion for this vascular disease.
One of the most prescribed treatments due to its being a standard of care for chronic venous insufficiency is compression therapy. This works by providing a pressure gradient of 30-40 mmHg between foot and knee to facilitate the venous return towards the heart and not reflux downward back to the foot to prevent the exacerbation of venous ulcers.
In line with this, it should be noted that there are various degrees of compression recommended for different conditions associated with chronic venous insufficiency, such as the following:
| Degree Of CompressionIndication<20 mmHgPrevention of deep vein thrombosis (graduated compression stocking)Mild edemaTired, aching legs (occupational leg symptoms20-30 mmHgMild varicose veinsMild to moderate edemaLong haul flights (>4 hours, high-risk patients for deep vein thrombosis)Varicose veins during and after pregnancy30-40 mmHgVenous ulcers (including healed ulcers)Deep vein thrombosisSuperficial thrombophlebitisFollowing venous surgery and sclerotherapyVaricose veins with severe edema and/or skin changesPost-thrombotic syndromeMild lymphedema>40 mmHgSevere lymphedemaSevere chronic venous insufficiency |
Before the initial treatment of compression therapy in patients with chronic venous insufficiency, however, accurate measurement on the ankle-brachial index through a Doppler should be done to determine if there’s an arterial disease that coexists with CVI. This gives a better idea of whether or not the compression therapy should be proceeded or withheld.
Compression therapy also has preventive effects in that it can decrease the rate of ulcer recurrence so it’s also dubbed as the standard of care for venous ulcer treatment. It helps hasten venous ulcer healing, encouraging the formation of granulation tissue and fibrin.
Types Of Compression Systems
Compression systems may be divided into inelastic compression therapy that has low pressure at rest and high pressure at work; elastic systems that have high pressure both at rest and at work; single layer with constant pressure; and multilayer that delivers a graded degree of compression.
Similarly, compression systems may further be classified into high-compression systems, support systems, and low-compression systems.
1) High-Compression Systems
Under the high-compression systems are the high-compression, multicomponent systems, and the high-compression, long stretch bandages, which differ on the materials and the way they work.
- High-compression, multicomponent systems – This type of compression system features 4 components namely natural padding and 3 bandages which can be described as light and flexible. This can’t be used with patients that have Doppler ABI values of <0.80, or those who have a coexisting arterial disease.
- High-compression, long stretch bandages – Long-stretch bandages feature 2 components namely orthopedic wool and a long-stretch elastic bandage. It’s more advantageous than multicomponent systems because they’re reusable, less bulky, and can be frequently inspected. They, however, have the tendency to slip off the patient’s legs.
2) Support Systems
Under the support systems category are the short-stretch bandages and the modified Unna boot which are classified as such because of the little elastic energy they possess.
- Support systems with short-stretch bandages – This support system works by opposing the expansion of the leg muscles when they contract. This helps venous blood return back to the heart instead of flowing backward away from the heart.
- Modified Unna boot – Modified Unna boot or paste bandage is a support system with a zinc-oxide gel covering an elastic gauze fabric, which, upon drying, serves as resistance against muscle contraction to facilitate venous blood return to the heart.
3) Low-Compression Systems
Under the low-compression systems are the single-layer elastic bandage and short-stretch system without underlayer. These compression systems are used for patients with an ABI between 0.6 and 0.8, meaning they have both arterial disease and venous disease.
The external pneumatic compression pump is a device under the low-compression system which is applicable for patients with uncontrolled edema or those patients who can’t tolerate the use of compression bandages.
Available Compression Therapy Materials
Some available materials that can be used in the management of compression therapy in patients with CVI and lower extremity ulcers include compression bandages, compression stockings, self-adjustable fabric hook and loop fastener devices, intermittent pneumatic compression pumps, and hybrid devices.
1) Compression Bandages
Compression bandages can be applied through different methods which don’t have evidence of a significant difference in their effect on the legs. These methods include spiral, continuous, or figure of eight.
Mostly used for the management of edema and venous stasis ulcers, compression bandages work best when done in the therapy phase. It’s useful for patients with fragile skin and those who can’t tolerate the effects of compression stockings.
Disadvantages of this procedure include the differences in the degree of compression even when administered by an experienced health care provider, poor compliance due to discomfort, and limitations in daily activities.
2) Compression Stockings
Medical compression stockings for patients with chronic venous insufficiency work through different compression grades, with the maximum compression pressure at the ankle and with decreasing pressure as it goes higher up the lower limbs.
Elastic stockings differ in the materials they’re made from. They may be made of silk, cotton, or nylon, which are then wrapped in elastic material. They may also be made of different styles, such as panty style, or above or below the knee.
It’s advantageous in that the compression grades of this garment don’t rely on the person applying it. However, the pressure profiles of stockings aren’t standardized and are made differently around the world. Patient compliance is also a problem possibly because of discomfort and aesthetic reasons.
3) Intermittent Pneumatic Compression Pumps
Intermittent pneumatic compression pumps are airtight chambers that work by mimicking the calf pump action in a normal limb, providing normal venous pressure that can help in increasing arterial flow, reducing edema, and managing venous return.
It’s applicable to those with unmanageable edema, those with peripheral artery disease, and those who can’t tolerate the level of compression provided by the other methods of compression. Its disadvantages, however, include its being expensive, bulky, noisy, and its need for a power source.
Other Ways To Manage Chronic Venous Insufficiency

The medical management of chronic venous insufficiency may also be facilitated with other methods such as diet and lifestyle modification, pharmacologic management, surgical management, and the use of aminaftone, an investigational drug.
1) Diet and Lifestyle
Diet and lifestyle modification may be considered as the initial treatment for chronic venous insufficiency. This includes maintaining a healthy weight through regular exercise since obesity is a risk factor for the exacerbation of chronic venous insufficiency. Raising the feet up to the level of the heart for 30 minutes at least 3 to 4 times a day and the prevention of prolonged standing and sitting help, too.
2) Pharmacologic Treatment
Pharmacologic treatment may be employed in patients with chronic venous insufficiency in order to help manage their symptoms such as edema, dermatitis, and infections. These include the following:
- Diuretics – Diuretics such as hydrochlorothiazide and furosemide, at low doses, may be used to treat the massive edema that patients with CVI may suffer from.
- Topical steroid cream or ointments – Topical steroid cream or ointments may be used to reduce skin inflammation. Fluocinolone or triamcinolone may be used for this purpose. Note that if these don’t work, the patients should be tested for contact dermatitis.
- Antibiotics – Antibiotics with the proper prescription of your health care provider are used to manage infections for those who already have cellulitis or infected chronic leg ulcer.
- Herbal Supplements – Herbal supplements with venoactive properties may also help in facilitating the reduction of edema, faster healing of venous leg ulcers, and reduction of inflammation associated with CVI. These herbal supplements include horse chestnut seed extract and micronized purified flavonoid fraction, among others.
3) Surgical Management
Surgical treatment may also be considered as an option for patients with recurring CVI. This may also be an option for those who want the prevention of ulcer recurrence. Surgical patients may undergo the following treatments:
- Veno-venous bypass (Palma’s procedure)
- Endovenous angioplasty
- Iliac vein stenting
- Ligation and stripping of varicose veins or phlebectomy
- Subfascial endoscopic perforator surgery
- Valve reconstruction or valvuloplasty
4) Aminaftone
Clinical trials show promise in the use of aminaftone as an emerging therapy for chronic venous insufficiency. It’s a useful oral medication for patients in the late stages of CVI, reducing symptoms such as edema, pain, cramps, itching, and heaviness.
Excellent Outpatient Vein Treatments at Vein Center Doctor

At Vein Center Doctor, we offer compression therapy for our patients that want to experience the best standard of care treatment backed with high-quality evidence on safety and efficiency. This treatment may also be supplemented with other excellent outpatient vein treatments that we offer to improve venous disorders of the leg veins, such as radiofrequency ablation, endovenous laser treatment, sclerotherapy, and VenaSeal Closure System. These managements may be considered as alternative therapies as well.
1) Radiofrequency Ablation
Radiofrequency ablation facilitates the improvement of signs and symptoms of venous incompetence through the obliteration of the endothelium, the inner lining of the target blood vessel. This procedure requires only local anesthesia instead of regional anesthesia.
Radiofrequency ablation is a kind of interventional treatment that uses radiofrequency delivered through a heat-tipped catheter that closes off the dilated vein so the blood flow will redirect to healthy veins. Since it’s minimally invasive, it’s ensured that it has minimal downtime, although compressive stockings or other garments must be worn to avoid adverse effects associated with the procedure, such as bruising and tenderness.
2) Endovenous Laser Treatment
Endovenous laser treatment is another kind of interventional treatment against chronic venous insufficiency which also works through the redirection of blood flow to normal veins. Through a heat-tipped catheter, it delivers a laser beam with wavelengths of 810-nm or 940-nm to close off the incompetent vein. Similar to RFA, endovenous laser treatment also has minimal downtime with mild side effects such as bruising and tenderness.
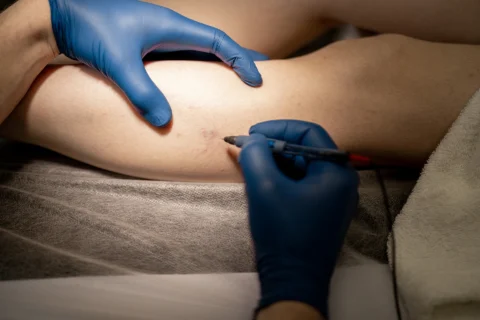
3) Sclerotherapy
Sclerotherapy also involves the closing off of incompetent veins but instead of heating, it involves the administration of chemicals called sclerosing agents. These sclerosing agents include 23.4% sodium chloride, sodium tetradecyl sulfate, and sodium iodide which irritate the endothelium to encourage inflammation and form scar tissue.
Two types of the procedure may be given by a healthcare provider, which include liquid sclerotherapy and ultrasound-guided foam sclerotherapy. The latter showed better efficacy because it isn’t diluted when administered, although it’s more painful than the former. Side effects associated with both types of sclerotherapy include thrombophlebitis and hyperpigmentation.
4) VenaSeal Closure System
The VenaSeal closure system is a minimally invasive procedure that involves the delivery of VenaSeal adhesive through a delivery catheter. This procedure uses ultrasound to visualize the access site and the delivery of the VenaSeal adhesive.
This procedure is done first by flushing with a saline solution followed by the specific sequence of delivery of the adhesive where it’s delivered every 3 cm for 3 seconds until all of the lengths of the target vein are covered. Compression of the area followed by bandaging the insertion site is then done to signal the end of the procedure.
Solve Your Vein Problems With Outpatient Vein Treatments at Vein Center Doctor
Compression therapy, with its different forms, can’t correct chronic venous insufficiency. However, its status as the standard of care for CVI and venous leg ulcers stems from the fact that it’s capable of bringing improvements to the signs and symptoms of the disorder and facilitating faster healing.
At Vein Center Doctor, we can help give the best clinical recommendations on managing the signs and symptoms of your vascular diseases with the excellent outpatient vein treatments that we offer. Our team, headed by Dr. Rahul Sood, is composed of healthcare professionals that are the best in their field, giving the guarantee that our procedures are safe and effective. Contact us today for your free consultation.