Navigating the causes, diagnosis, and treatments of telangiectasia on the nose can help you regain confidence in your skin.
Telangiectasia on the nose is caused by visible blood vessels near the skin’s surface.
Factors like genetics, sun exposure, rosacea, and hormonal changes can lead to this common skin condition.
To reduce the risk, it’s important to apply daily sunscreen, avoid harsh products, and wear a hat when outdoors.
Treatment options for telangiectasia on the nose include laser therapy and sclerotherapy.
If concerned about this issue, it’s essential to understand the underlying causes, diagnosis, and management strategies.
Key Takeaways
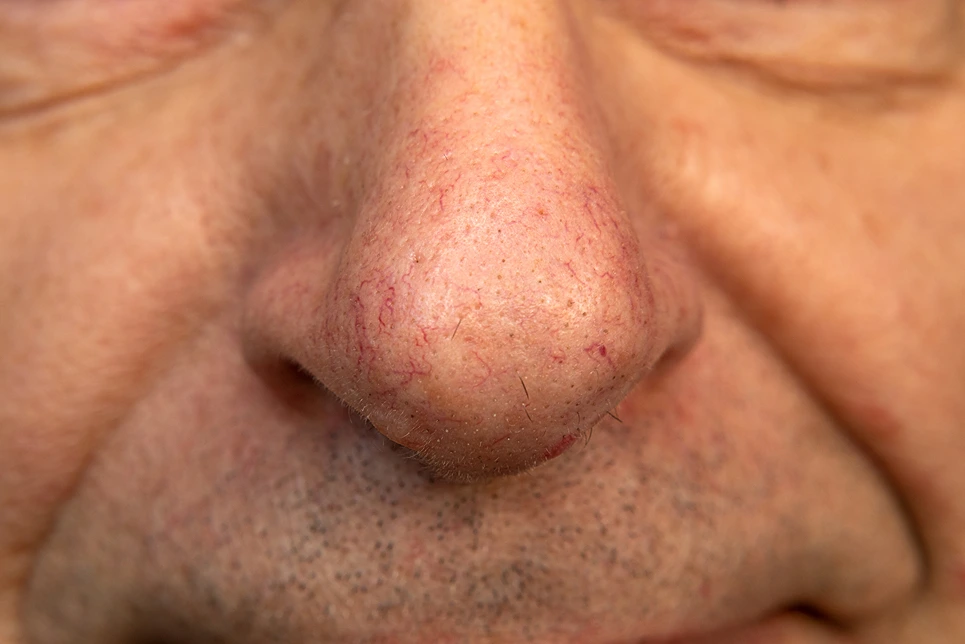
Telangiectasia on the nose is characterized by red, blue, or purple lines caused by visible blood vessels near the skin’s surface.
Causes: Genetic factors, sun exposure, rosacea, hormonal changes, and trauma can lead to telangiectasia. Family history and prolonged sun exposure increase the risk.
Diagnosis: Healthcare providers diagnose telangiectasia on the nose through visual assessment and a dermatoscope. It can be linked to skin conditions like rosacea, lupus, and scleroderma.
Treatment: A combination of laser therapy and sclerotherapy is effective for treating telangiectasia on the nose, targeting both small and larger blood vessels.
Management: Long-term management of telangiectasia involves regular dermatologist visits, daily sunscreen use, and gentle skincare routines. Additional treatments may be necessary as needed.
Understanding Telangiectasia
Telangiectasia on the nose presents as tiny, visible blood vessels due to dilation near the skin’s surface. This condition isn’t a disease but a result of skin changes. Recognizing telangiectasia is crucial for proper treatment.
Telangiectasia manifests as red, blue, or purple lines on the nose. The dilation of these small blood vessels causes the thread-like patterns you see. Addressing this skin condition involves understanding its signs and seeking appropriate care.
Causes and Risk Factors
- Telangiectasia on the nose can be caused by genetic factors, sun exposure, conditions like rosacea, hormonal changes, and trauma.
- Having a family history of telangiectasia increases the risk, as does prolonged sun exposure that damages the skin and dilates blood vessels.
- Rosacea, an underlying skin condition, is a common cause of telangiectasia.
- Hormonal changes such as those during pregnancy or menopause can also contribute to its development.
- Injury or surgery on the nose can trigger telangiectasia as well.
- To reduce the risk, it’s important to avoid excessive sun exposure, alcohol consumption, and manage conditions like rosacea.
Understanding these causes and risk factors is crucial for maintaining healthy skin free from telangiectasia on the nose.
Symptoms and Diagnosis

Visible blood vessels in the nose can appear as fine, red, blue, or purple lines. Nasal discoloration signs like redness or a bluish tint may also be noticed.
Healthcare providers use visual assessment and a dermatoscope to diagnose telangiectasia.
Visible Blood Vessels
Visible blood vessels on the nose are thin, red or purple lines that resemble a spider web. These vessels are a common sign of telangiectasia. They can be easily seen near the skin’s surface, causing concern for some individuals.
Visible blood vessels on the nose appear as fine, threadlike red or purple lines, creating a spider-like pattern.
Telangiectasia is a common cause of visible blood vessels on the nose. These blood vessels are dilated and close to the skin’s surface, making them noticeable.
Yes, visible blood vessels on the nose can be a cosmetic concern due to their prominent appearance.
Nasal Discoloration Signs
Nasal telangiectasia can lead to red or purple discoloration on the nose, caused by visible blood vessels. This condition is commonly associated with rosacea or sun damage.
Seek medical advice if you notice nasal discoloration or visible blood vessels on your nose. A doctor can visually identify telangiectasia during an examination.
Nasal telangiectasia may affect your appearance or cause discomfort.
Early diagnosis and treatment can help manage symptoms and improve the nose’s appearance. It’s essential to consult a doctor promptly if you observe any unusual nasal discoloration.
Diagnostic Procedures Used
Telangiectasia on the nose is typically diagnosed through visual examination, dermoscopy, and occasionally a skin biopsy.
- Visual examination involves a close inspection of the nose for visible red or blue blood vessels.
- Dermoscopy, which magnifies the skin, can aid in a more detailed examination.
- A skin biopsy may be recommended if the diagnosis remains unclear, allowing for microscopic analysis of a skin sample to differentiate telangiectasia from other skin conditions.
- Imaging tests may be used in some cases to rule out underlying issues or related skin disorders.
Connection to Skin Conditions
Skin conditions like rosacea, lupus, and scleroderma can lead to telangiectasia on the nose.
Rosacea is a skin condition that can cause chronic inflammation, leading to the development of telangiectasia on the nose.
Lupus is an autoimmune disease that may result in telangiectasia on the nose due to the body’s immune system attacking healthy tissue.
Scleroderma is a condition characterized by skin thickening and vascular damage, which can contribute to the formation of telangiectasia on the nose.
Consult a dermatologist for a proper diagnosis and treatment plan if you suspect an underlying skin condition causing telangiectasia on your nose. Effective management involves addressing the root skin condition.
Prevention and Self-Care

To reduce the appearance of telangiectasia on your nose and prevent further dilation of blood vessels, protecting and caring for your skin is crucial.
One essential step is applying SPF 30 broad-spectrum sunscreen daily to shield your nose from harmful UV rays.
Avoid using harsh facial cleansers and irritating products that can worsen telangiectasia, opting instead for gentle skincare suitable for sensitive skin.
Wearing a wide-brimmed hat when outdoors can also protect your nose from direct sunlight.
Maintaining a healthy lifestyle with a balanced diet and regular exercise supports overall skin health.
Treatment Options Explained
Telangiectasia on your nose can be effectively treated with laser therapy and sclerotherapy. Laser therapy targets and shrinks broken blood vessels, while sclerotherapy involves injecting a solution into the vessels. Both treatments offer long-lasting results and require consultation with a dermatologist for the best outcome.
After treatment, it’s crucial to prioritize sun protection to prevent telangiectasia recurrence. By following these steps and seeking professional advice, you can successfully address telangiectasia on your nose and maintain healthy, radiant skin.
Laser Therapy and Sclerotherapy
Laser therapy and sclerotherapy are common treatments for telangiectasia on the nose. Laser therapy shrinks and seals off blood vessels using heat, while sclerotherapy involves injecting a solution to harden and eliminate the vessels.
For example, in laser therapy, a focused beam of light targets the blood vessels, causing them to shrink and eventually disappear.
In sclerotherapy, a solution is injected into the vessels, irritating the lining and causing them to collapse and be reabsorbed by the body.
Understanding these treatments can help you decide which option is best for treating telangiectasia on your nose.
How Laser Therapy Works
Laser therapy for telangiectasia on the nose works by targeting dilated blood vessels with precision. The laser emits a specific wavelength of light that heats up and shrinks the affected blood vessels.
Benefits of laser therapy for telangiectasia on the nose:
- Minimally invasive: It’s a quick and relatively painless treatment.
- High success rate: Laser therapy is highly effective in completely removing telangiectasia on the nose.
- Quick recovery time: Patients can resume normal activities shortly after treatment.
- Targeted treatment: The laser focuses only on the affected areas, leaving surrounding skin untouched.
- Long-term results: Proper treatment can lead to long-lasting outcomes.
Sclerotherapy Treatment Options
Sclerotherapy is a treatment option for nose telangiectasia that involves injecting a solution into the affected blood vessel to harden and eliminate it. Unlike laser therapy, which uses heat, sclerotherapy directly targets and treats the vessel.
The procedure may cause a slight stinging sensation during the injection, with possible mild and temporary side effects like bruising, swelling, or redness afterwards. Your dermatologist will ensure your comfort throughout the process.
Consult with a dermatologist to determine the best treatment for your nose telangiectasia. They’ll assess the condition and recommend sclerotherapy, laser therapy, or a combination based on your specific needs.
Combining Treatment Methods
Combining laser therapy and sclerotherapy is an effective way to treat telangiectasia on the nose. Laser therapy targets smaller blood vessels, while sclerotherapy treats larger veins. This combination approach ensures complete removal of telangiectasia by addressing a range of blood vessel sizes.
Benefits of combining laser therapy and sclerotherapy for treating telangiectasia on the nose include:
- Targeting small blood vessels with laser therapy.
- Treating larger veins with sclerotherapy.
- Improving the appearance of fine blood vessels with laser therapy.
- Achieving more thorough results through combination therapy.
This dual treatment method leverages the strengths of each approach to provide comprehensive treatment for telangiectasia on the nose.
What to Expect From Doctors
When you see a doctor for telangiectasia on your nose, they’ll visually examine the area to assess the condition’s severity. This helps in determining the appropriate treatment.
Your doctor may suggest blood tests or imaging studies to rule out underlying causes linked to telangiectasia. These tests assist in identifying any contributing factors that require attention.
Treatment options such as laser therapy or sclerotherapy may be discussed based on the size and location of the telangiectasia. Laser therapy uses light to target blood vessels, while sclerotherapy involves injecting a solution to shrink them.
Feel free to ask questions or share any concerns during the consultation. Your doctor is there to provide support and guidance regarding your telangiectasia.
Managing Telangiectasia Long-Term

Effective long-term management of telangiectasia on the nose involves regular dermatologist visits, sun protection, and a consistent skincare routine.
- Regular Dermatologist Visits: Schedule routine appointments to monitor telangiectasia progression.
- Sun Protection: Use SPF 30 sunscreen daily, reapply every two hours, and wear hats or seek shade to shield the nose from harmful UV rays.
- Skincare Routine: Employ gentle, hydrating products to maintain skin health and hydration, preventing further damage.
- Avoid Triggers: Steer clear of alcohol and extreme temperatures that can worsen telangiectasia.
- Consider Laser Therapy: Opt for additional treatments like laser therapy if needed for optimal results.
Conclusion
Telangiectasia on the nose can be managed effectively with the right approach. Understanding the causes is crucial. Tiny blood vessels near the surface of the skin become dilated, resulting in the appearance of red or purple lines.
Symptoms include redness, visible blood vessels, and sometimes a flushed appearance. Treatment options range from laser therapy to topical creams.
Laser therapy targets and shrinks the blood vessels, reducing their appearance. Topical creams can help improve skin texture and reduce redness.
Consistency in treatment and diligent skincare are key to managing telangiectasia on the nose.







