Explore the causes and symptoms of spider veins and discover effective modern treatments to reduce and eliminate these vein issues.
What Are Spider Veins?

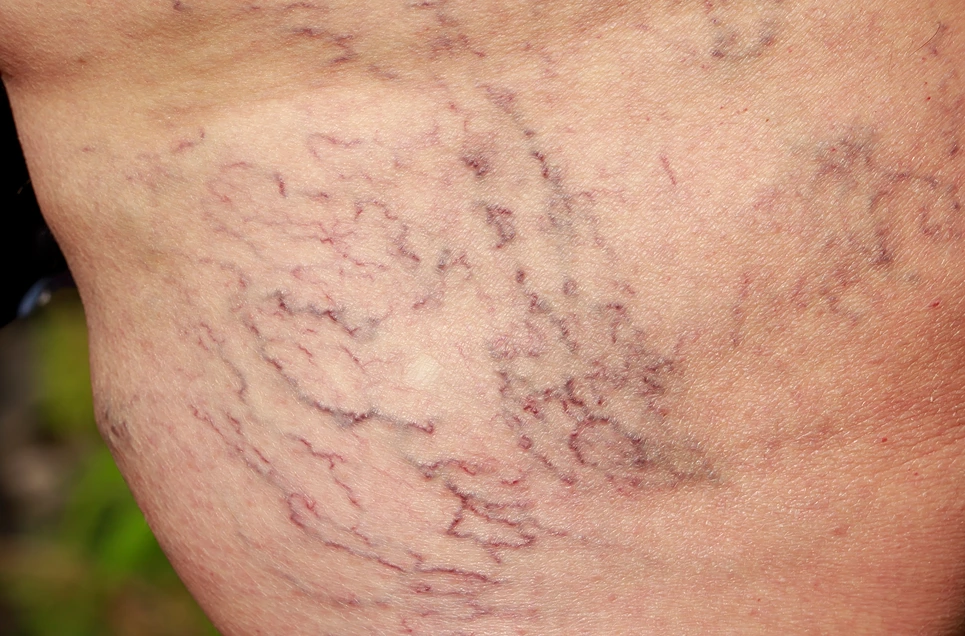
Spider veins are small, thin veins close to the skin surface, often red or blue with a web-like or branched appearance.
They can appear anywhere on the body, but are most common on the legs and face.
What Causes Spider Veins?
Spider veins develop due to factors affecting the circulatory system, particularly the veins’ ability to transport blood back to the heart.
What Are Collapsing Spider Veins?
When spider veins collapse, it means they’ve been treated, usually through sclerotherapy, causing them to spasm and collapse.
Over time, the walls of the collapsed vein heal together, and the sealed vein can no longer carry blood.
Venous Pressure and Valve Malfunction
Veins have one-way valves for upward blood flow to the heart. When these valves weaken or are damaged, blood can flow backward, causing pressure buildup. Increased pressure weakens and bulges vein walls, making spider veins more visible.
Genetic Predisposition
A family history increases the likelihood of developing spider veins.
Age
The risk of spider veins increases with age as vein valves can weaken over time.
Occupational Risks
Jobs requiring prolonged standing can put pressure on leg veins, contributing to the development of spider veins.
Hormonal Changes
Hormonal fluctuations, like during pregnancy or due to estrogen levels, can cause spider veins by dilating the veins.
Lifestyle Factors
Obesity, lack of exercise, and prolonged sitting or standing contribute to spider veins.
Sun Exposure
Sun damage causes spider veins, especially on the face.
Other Factors
Past injuries, blood clots, or VTE can increase the risk of spider veins in the affected limb.
What Are the Symptoms of Spider Veins?
The most common spider vein symptoms are:
- Leg aching or fatigue due to improper vein function can cause discomfort when standing or walking.
- Leg heaviness or swelling can be caused by poorly functioning veins struggling to pump blood back to the heart, causing blood to pool in the legs.
- Itching or tingling of the skin is caused by minor irritation or inflammation from damaged veins just under the skin’s surface.
- Spider veins are small red, blue, or purple lines under the skin. Though not painful, some people want to improve their appearance.
Spider veins are usually not very painful, but can cause fatigue, heaviness, aching and swelling in the legs of multiple veins.
Seeking treatment from a dermatologist or vascular surgeon can help address the root cause and relieve symptoms.
Medical Process Behind the Collapse of Spider Veins

Spider vein collapse is often the result of medical treatments that aim to close off the affected veins, causing them to shrink and become less visible:
- Sclerotherapy – This involves injecting a solution into the vein to irritate the vein walls, causing them to collapse and scar over.
- Laser and Intense Pulse Light Therapy (IPLT) – These non-invasive treatments use light energy to heat and damage the vein, causing it to collapse.
- Vein Ablation – A minimally invasive procedure that uses heat to close off affected veins.
- Microphlebectomy – A technique that involves removing the vein through small incisions or needle punctures.
- Compression Therapy – Wearing medical-grade compression stockings can improve circulation, reduce venous pressure, prevent spider veins, and reduce symptoms.
- Physical and Occupational Therapy – These therapies may complement other treatments and address lifestyle factors causing spider veins.
How Common Are Collapsing Spider Veins?
Spider veins are common, with about one-third of adults having some form of venous disease.
Spider veins are more likely with age and more common in cisgender women than in cisgender men.
The treatment and collapse of spider veins is common, as people seek treatment for cosmetic or discomfort reasons.
What Is the Medical Process Behind the Collapse of Spider Veins?
The medical process behind the collapse of spider veins is typically sclerotherapy.
In this procedure, a healthcare provider injects a sclerosant into the affected vein, causing it to spasm and collapse.
Over time, the walls of the collapsed vein heal together, sealing it off and stopping blood flow. The body naturally reroutes blood to healthier veins.
Over time, the treated spider veins fade as the body reabsorbs the collapsed vein.
How Does Age Affect the Likelihood of Spider Veins Collapsing?
Age is a significant factor in the development of spider veins. As we age, wear and tear on the vein valves increases, leading to the formation of spider veins.
Varicose veins are more likely as veins weaken with age, due to weakened or damaged one-way valves causing blood to pool and the veins to become swollen and twisted.
The older you are, the more likely you are to develop spider veins that may need treatment and collapse.
What Role Does Genetics Play in the Development and Collapse of Spider Veins?
Genetics significantly influences spider vein development. If your parents have them, you’re likely to develop them too.
Varicose veins, similar to spider veins but larger and more symptomatic, are more common in those with a parent’s history, increasing the probability by 40-90%.
If spider veins run in your family, you may be more likely to develop them and need treatment for their collapse.
How Do Lifestyle Factors Contribute to the Collapse of Spider Veins?
Lifestyle factors can significantly contribute to the development and collapse of spider veins.
- Being overweight or obese can increase the risk of developing spider veins due to the extra pressure on the veins.
- Standing for long periods at work may increase the likelihood of developing spider veins. Regular physical activity, especially leg muscle exercises, can help prevent new spider veins.
- Maintaining a healthy weight and staying active can help prevent the development of spider veins that may need treatment.
How Do Collapsing Spider Veins Differ From Varicose Veins?
Spider veins and varicose veins are types of venous disease, but they differ in size, appearance, and symptoms.
Spider veins are small, close to the skin surface, and usually red or blue. They typically appear on the legs or face and don’t bulge out.
Varicose veins are larger, dark purple or blue, and appear twisted and bulging, like cords on the legs.
Both conditions can be treated with sclerotherapy, but varicose veins have more severe symptoms and cosmetic concerns.
What Distinguishes Collapsing Spider Veins From Other Vascular Conditions?
The main feature of spider veins compared to other vascular conditions is their small size and superficial location in the legs.
- Spider veins are very small, thin blood vessels usually less than 1 mm in diameter, located in the superficial dermis layer of skin.
- Varicose veins involve larger, twisted veins deeper in the legs, often greater than 3 mm in diameter.
- Spider veins have a spider-like or thread-like appearance close to the skin, while varicose veins are raised, rope-like veins.
How Do Collapsing Spider Veins Affect a Person’s Overall Health?
Collapsing spider veins are primarily a cosmetic concern, but can indicate underlying circulatory issues like chronic venous insufficiency (CVI).
Spider veins usually don’t cause major health problems, but can lead to discomfort, especially if they indicate a more significant venous condition. If they are symptomatic of CVI, they could lead to serious complications if untreated.
What Are the Current Treatment Options for Collapsing Spider Veins?
The most common treatment for collapsing spider veins is sclerotherapy, a procedure where a solution is injected into the veins to make them shrink and disappear.
Laser treatments are available, involving directing concentrated light beams at the veins to destroy them. Both treatments are minimally invasive and can be done in an office.
How Effective Are Non-Surgical Treatments for Collapsing Spider Veins?
Non-surgical treatments like sclerotherapy and laser therapy are effective for collapsing spider veins.
Most patients see at least a 50% improvement with one sclerotherapy treatment, and some see total eradication of their spider veins. Laser treatments also have a high success rate, but effectiveness can vary based on the individual case.
What Are Some Common Misconceptions About Collapsing Spider Veins?
A common misconception about collapsing spider veins is that they are always harmful or indicative of a serious health issue. While they can be associated with underlying conditions, spider veins themselves are not usually harmful.
Treatment isn’t always necessary; many people opt for it for cosmetic rather than health reasons.
Conclusion

Collapsing spider veins are usually a cosmetic issue but can indicate underlying venous conditions.
Sclerotherapy and laser therapy are effective for most individuals, but not necessary for everyone.
Understanding spider veins and available treatments helps individuals make informed decisions about their care.







